Estimated read time: 4-5 minutes
This archived news story is available only for your personal, non-commercial use. Information in the story may be outdated or superseded by additional information. Reading or replaying the story in its archived form does not constitute a republication of the story.
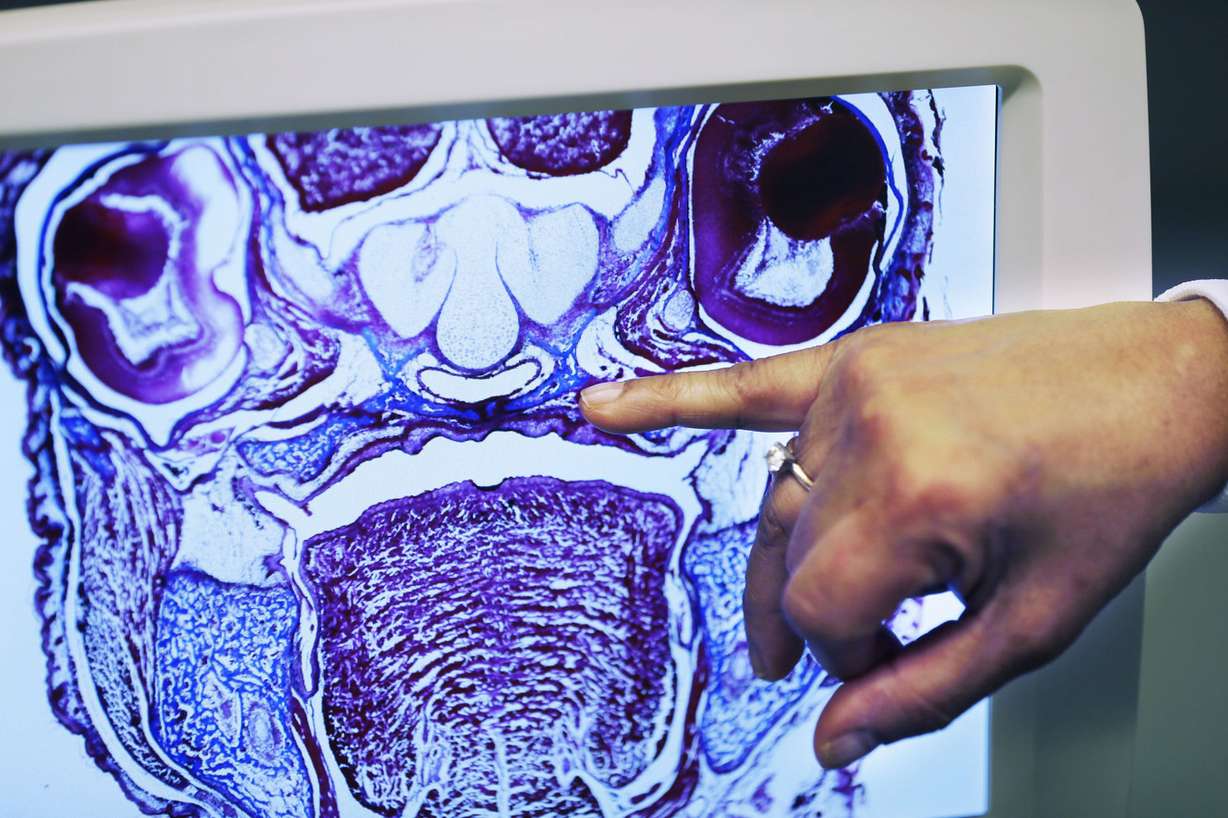
SALT LAKE CITY — Researchers at the University of Utah say they have identified how to reverse the cleft palate defect for mice still in the womb, potentially opening the door for similar treatment of unborn human babies in the future.
The cleft palates of all the tested unborn mice, or "pups," were successfully reversed and the treatment exhibited no side effects, said Dr. Rena D'Souza, a professor of dentistry at the U. and the lead author of the study, published Sept. 5 in the peer-reviewed scientific journal Development.
"I can't think of anything more gratifying than this," D'Souza told the Deseret News. "You don't always run into something that is contributing to advancing knowledge (in this) way."
D'Souza, who is also the incoming president of the International Association of Dental Research and practices dentistry clinically, said if a similar treatment can be made available to humans, the benefits would be remarkable.
"The only thing we can do right now, and have available, is surgery," she said. "Very often there are complications and you have to go back into repeated surgeries."
Cleft palate, a condition in which the sides of the roof of the mouth do not join together during fetal development, affects 1 in roughly 1,574 infants born in the United States, according to the Centers for Disease Control and Prevention.
Out of 22 common categories of birth defects listed online by the CDC, cleft palate's prevalence is the third-highest, trailing only cleft lip and Down syndrome.
The reversal was achieved through the use of a drug based on a gene called Wnt, D'Souza said.
Typically, a gene called PAX 9 helps sustain the activity of the Wnt gene, which is critical for fusion, but Pax 9's absence can allow such activity to be blocked by two genes that inhibit Wnt. That ultimately leads to a cleft palate.
The treatment is another way to activate Wnt activity by confronting the two genes that inhibit it, thus ensuring the proper fusion of the roof of the mouth. The test succeeded in bridging the palate in each tested case.
"We had a consistent closure of the cleft defect in utero," D'Souza said.
Excessive medical complications of living with a cleft palate affect numerous aspects of daily life, she said, "the way you swallow, the way you speak, the way you inhale." On top of those setbacks, "society places a stigma on individuals who don't look normal," D'Souza said.
"The face is such an important part of our identity," she said. "It gives us a sense of self-esteem and well-being and all of that."
However, much more work needs to be done to determine whether the treatment is feasible in humans, D'Souza said. One limitation is that cleft palate "is not always the result of a single gene misbehaving," she said, so any eventual treatment using the in-utero method would need to come after identifying the specific underlying reason for the malformation.
Another issue is the treatment's lack of an effect on other defects related to the absence of the PAX 9 gene, D'Souza said.
"Along with cleft defects, PAX 9 deficient pups also experience defects in their hind limb, as well as parathyroid and thymus glands. The Wnt-based treatment did not prevent the other defects, and the PAX 9-deficient pups soon died after birth," University of Utah Health Sciences writer Stacy Kish explained in a release.
The cause of those young pups' deaths is considered to be related to their initial genetic problems and is not a side effect of the treatment they received while in the uterus, D'Souza said. She added that the siblings of mice in the same uterus that didn't suffer from an absence of the PAX 9 gene and lived past birth showed no side effects from the treatment for the ensuing 18 months they were tracked.
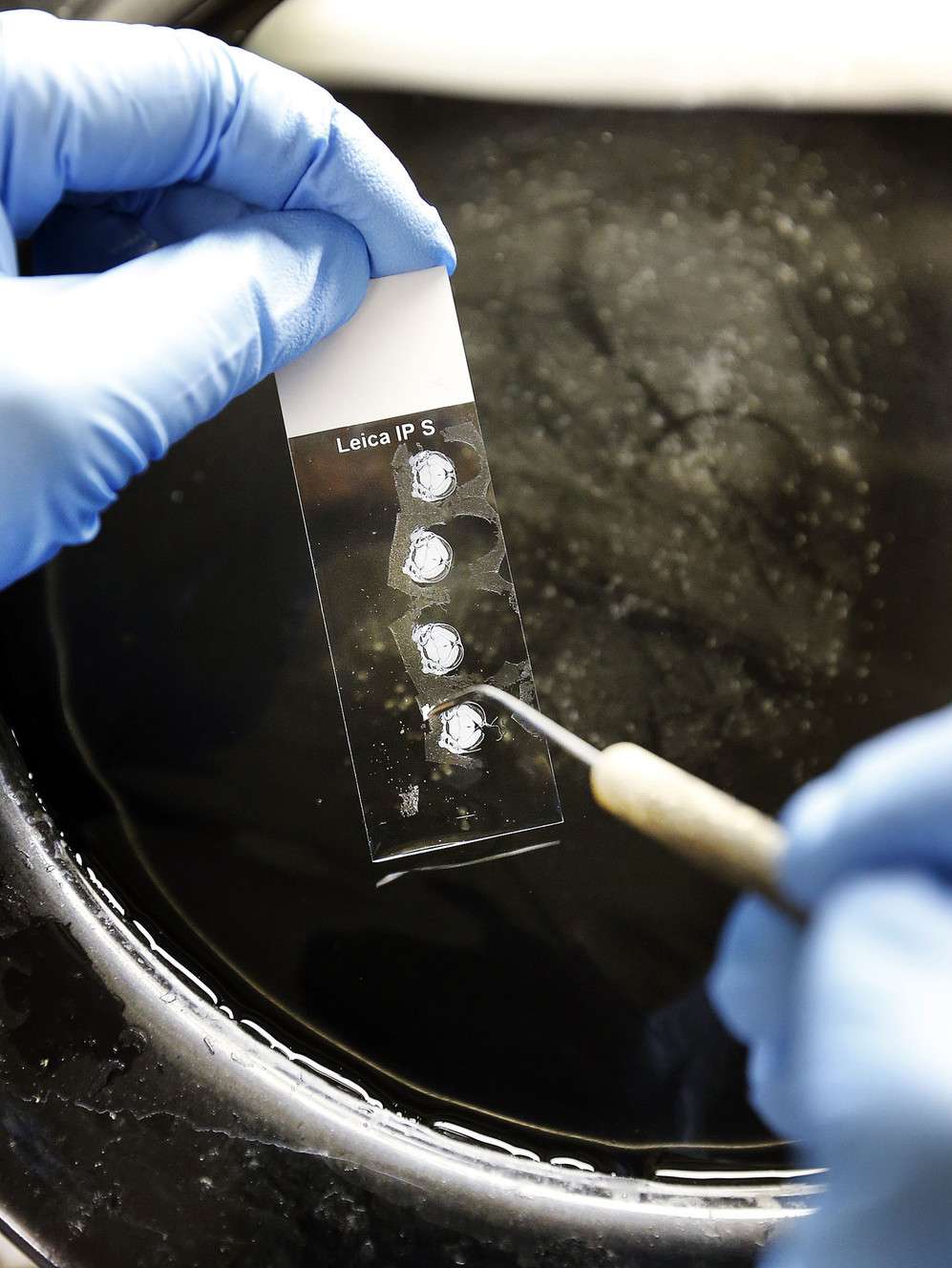
Their mothers, who had received the injection through the tail, also showed no side effects, D'Souza said.
"They were fine. There were no toxic defects, there were no tumors (or) anything you could think of," she said.
Despite the study not identifying side effects, more research needs to be done in that area, D'Souza added.
The discovery was praised by Dr. Ophir Klein, chief of genetics at the University of California, San Francisco. Klein was not an author in the study but said the findings may become a foothold in discovering how to undo the harms of similar defects.
"These seminal findings are exciting for the field," Klein said as part of a prepared statement.
D'Souza called her discovery "serendipitous," having arisen from an initial effort to understand the roles played by the Wnt and PAX 9 genes in the formation of teeth. She said she is eager to examine the implications for humans in the future.
"Since harsh surgeries are the only treatment options available, it is so critical to develop (noninvasive), safe and effective approaches to cure such a devastating genetic disorder," D'Souza said.
Researchers from the U., Texas A&M University and the University of Lausanne (Switzerland) contributed to the study. Funding for the research was granted by the Swiss National Science Foundation, as well as the National Institute of Dental and Craniofacial Research, which is part of the National Institutes of Health.








